AHI Blog
Posts from AHI students on Fordham's program, working in healthcare, and what is up and coming in Health Informatics.

The Role of Health Informatics in Responding to the Violence Against Black Trans Women
By Kerry Gilder

In 2022, the Human Rights Campaign reported that at least 44 transgender and gender non-conforming people were killed in the U.S., and over half were Black transgender women. Violence against Black transgender women is a serious public health and social justice issue. This population is uniquely vulnerable due to systemic racism, misogyny, and transphobia, creating disproportionate levels of violence and discrimination.
The violence experienced by Black trans women has health implications beyond injury and mortality, including but not limited to mental health issues like anxiety, depression, and PTSD. Effective health informatics can provide the tools necessary to understand and address the rates of these disorders, as well as to track violence for early detection of outbreaks in the areas where these women live. Enhanced data analysis can be very useful—however, this also means enhanced data collection, which needs to be done safely.

Here are some applications of health informatics for this at-risk population:
- Health Information Systems: Using information systems to capture data on violence. Data could be anonymized separately from medical records, alleviating fears about reporting. Example: In the 1980s, anonymous HIV reporting helped identify outbreak hotspots allowing for interventions while still maintaining privacy.
- Enhanced Electronic Health Records (EHRs): Modifying EHRs to capture self-reported gender identity and experiences of violence. This can help implement more appropriately focused interventions and support.
Example: Enhanced EHRs have been used to better track the health of LGBTQIA+ populations, leading to more specialized care. Capturing gender identity in EHRs has led to more gender affirming psychosocial care.
- Public Health Surveillance: Collecting and analyzing public health data, shared with consent, to implement best practices.
Example: Public health surveillance could help begin to mitigate the epidemic of violence against Black trans women.
- Predictive Analytics: Tracking and monitoring trends and outbreaks of violence across geographic areas. This can inform strategies and resource allocation.
Example: Enabling the tracking of movement patterns of the perpetrators of these attacks leading to preventive measures.
- Telehealth Services: Enabling access to mental health support, medical consultation, and follow-up care. Especially for those who feel unsafe going to a facility or in remote and underserved areas.
Example: Telehealth Services have taken off since the Covid-19 pandemic allowing many who would not otherwise have had access to receive the care they needed.
- Culturally Competent Care: Designing more training programs for healthcare providers to learn about the care methods that address the unique social and experiential needs of Black trans women. It should also be noted that better equipped clinicians can lead to more data collection and reporting.
Example: Cultural competency through Blue Cross Blue Shield Minnesota offers training in depression management specific to different races and ethnicities. These resources have helped improve adherence to antidepressant medications and treatment. 
However, the power of health informatics comes with risks:
- Privacy Concerns It is of the utmost importance that patients' information is kept confidential to prevent its misuse, examples of which could lead to further discrimination and violence. Anonymizing data collection can provide necessary protection.
- Data Security An even more emphatic need for measures in cybersecurity exists, especially against data breaches.
- Informed Consent These women must be well-informed on how their information is going to be used and be provided with the right to opt out of data collection.
Community advocacy and involvement is a base requirement. Black trans women should be part of the discussion surrounding health surveillance for their perspectives to be foundational in the creation of the above approaches and their implementation.
In conclusion, health informatics offers tools to address violence and health disparities experienced by the Black trans population. The benefits here should be weighed against the risks. Discussions surrounding the health of a marginalized group should always consider the perspectives of the demographic to have their needs and perspectives met.
Kerry Gilder is a CASAC-T certified addiction counselor and student in the AHI masters program at Fordham University, where she combines her passions for psychology, computers, and helping people in crisis.
Guide to Creating AI-Assisted UML for Care Pathway Diagrams in Behavioral Health

By Kerry Gilder
Introduction
Artificial Intelligence (AI) can enhance how we design systems to manage healthcare processes. This post explores how AI tools help create Unified Modeling Language (UML) diagrams to visualize these processes, making it easier to understand and manage patient care. UML is a standard way to visualize system designs for software developers. It can also be used to generate workflows and other diagrams. Two AI tools were compared for creating UML diagrams are:
- ChatUML™, A chatbot that helps generate UML diagrams through interactive dialogues.
- OpenAI™, Used to write and execute code, helping in the diagram creation process.
In the case referenced below, both OpenAI™ and ChatUML™ use PlantUML, a tool that allows users to create UML diagrams from plain text descriptions.
Methods
Both tools were tested for their effectiveness in creating accurate and efficient UML diagrams. For ChatUML™, we engaged in conversation with the chatbot to generate diagrams. With OpenAI™, we used AI to directly provide the PlantUML script and separately executed it to produce diagrams.
Results
OpenAI™ was found to be more effective at generating precise UML diagrams through measured differences and more attuned questions for the clinicians were noted. Here are key distinctions:
|
Criteria |
ChatUML™ |
OpenAI™ |
|
Ease of Use |
Extensive |
Moderate |
|
Control Over Details |
Limited |
Extensive |
|
Accuracy of Diagrams |
Moderate |
Extensive |
|
Time Efficiency |
Moderate |
Extensive |
Below is the code and a simple AI-generated diagram for a serious mental health (SMI) crisis management use case:
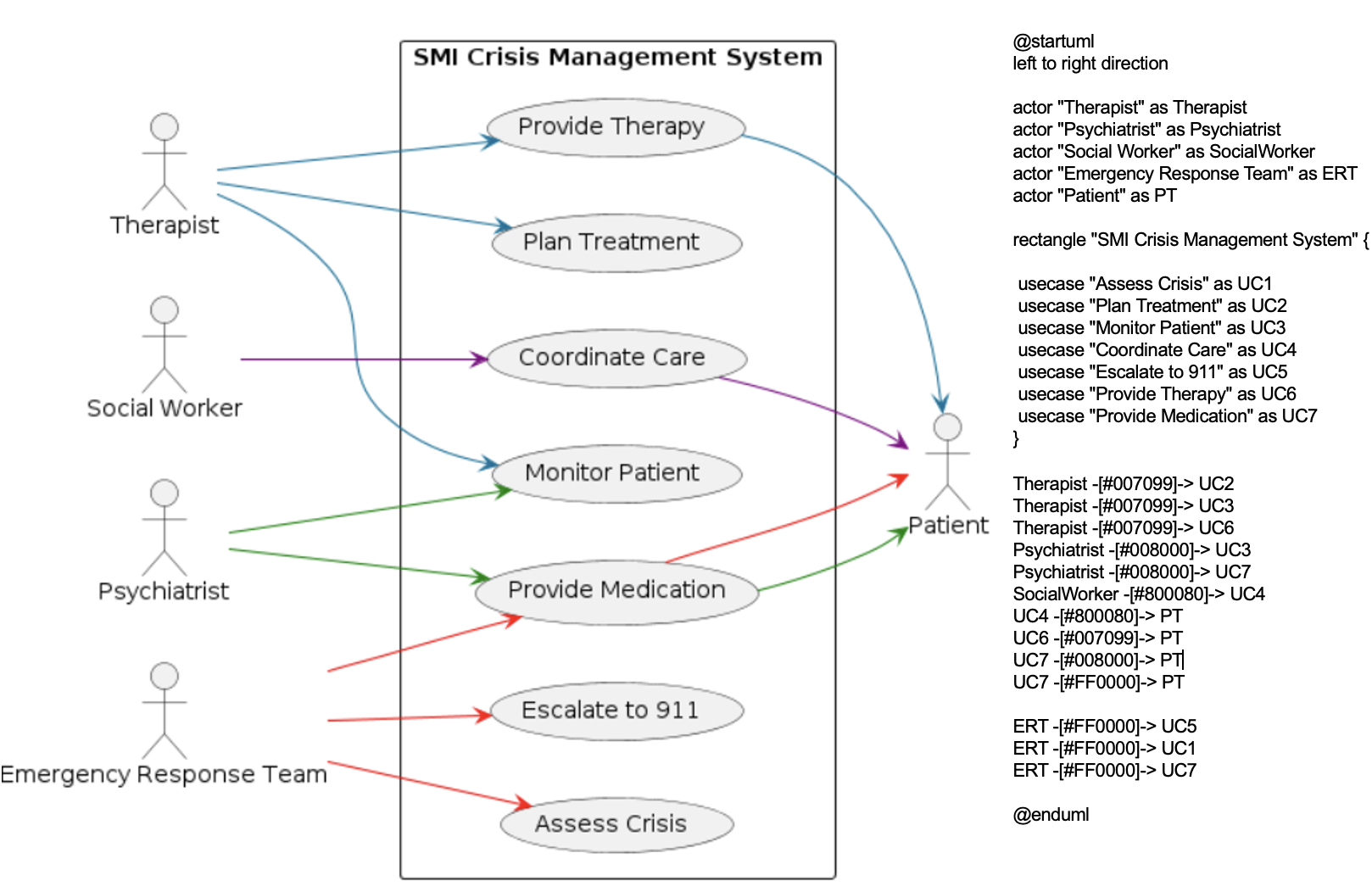
Value to Potential Users
These AI tools make the process more accessible and efficient for healthcare professionals, who might not have the background to write code. Above is the practical application of an AI-generated diagram in mental health crises, demonstrating their effectiveness in real-world scenarios. Assistants producing PlantUML with the help of an OpenAI™ assistant can benefit the psychiatrist, therapist, social worker, emergency response team, and patient in various ways beyond just the flow of care. Some examples of this are highlighted below:
|
Psychiatrist |
Creation of AI-generated UML diagrams to clearly understand patient histories, treatment plans, and mental health assessments, facilitating more accurate diagnoses and personalized treatment strategies. |
|
Therapist |
Progress tracking, and patient feedback through diagrams, aiding in developing new approaches and improving treatment outcomes. |
|
Social Worker |
Structure case management diagrams outlining patient support systems and resources, enabling them to provide more comprehensive and coordinated care. |
|
Emergency Response Team |
Real-time, AI-generated simulations to prepare for mental health crises, ensuring quick and coordinated responses during emergencies. |
|
Patient |
Receive clear, visual representations of treatment plans and progress, helping them understand their mental health and participate in their care. |
Conclusion
Using AI to create UML diagrams can improve the design and management of healthcare systems. These tools enhance speed and efficiency; however, specialists’ expertise remains crucial for validation. Continued development in AI tools will further improve their accuracy and usability, benefiting both the providers and the patients. AI serves as a useful assistant, streamlining the design process and making healthcare providers more agile in using these tools.
Kerry Gilder is a CASAC-T certified addiction counselor and student in the AHI masters program at Fordham University, where she combines her passions for psychology, computers, and helping people in crisis.
From the Operating Room to the Server Room: One Nurse's Journey of Growth in Health Informatics
By Imelda Soledad, RDH, RN, BSN, BMTCN.
I am a nurse who strives to continuously learn and adapt to the latest technologies. As technological advancements have continued to develop at an astonishing rate at my hospital, I started to look seriously into making a mid-career change more focused on the interface of information flow and healthcare delivery. The field of Health Informatics caught my attention when I met my first Nurse Informaticist. I then considered it as a future career goal.
While doing my research, I came across a program in Fordham and ever since then my life has forever changed.
I never thought that I will find myself studying again after more than a decade of completing my second college degree in nursing. I love to study and gain new knowledge that I can use to be a better nurse and person. When I started working as a nurse, the busy schedules and workloads occupied so much of my time, and my passion for studying ended up on the back burner. The flexible nature of Fordham's AHI coursework gave me the opportunity to study again.
Initially I was skeptical that I had the technical background to do well. I decided to reach out to Dr. Chelsom, the director of the program. He is very approachable, caring and accommodating. I was connected to a previous student, who was very helpful in assuaging my fears. She gave me moral support and a better sense about what the program entails, including how she balanced taking care of small children while doing the course online.
Dr. Chelsom and the AHI faculty have been very considerate and supportive to me. They offer one on one tutoring and support through zoom meetings when I request it, and work around my schedule. They would also give suggestions and have guided me to discover talents that I never knew I have.

One of the highlights of this program was the chance to study in Oxford. It was an amazing experience — getting to know more people and learning about new cultures. To be in a room with different students coming from different parts of the world was in itself an exciting experience. In addition, the program's curriculum in Oxford was exemplary- composed of talks from lecturers that were experienced, knowledgeable and friendly.
I had the opportunity for personal growth during this trip as well. Aside from my experience of Oxford University, I was able to stay one more week in London and did my first solo travel. Navigating the city on my own was unexpected and memorable.
The AHI program has taught me a lot and introduced me to lots of new and interesting people. I love the fact that even though we have different background and cultures, we are still connected by our passion to make healthcare better. The hybrid nature of the program offers flexibility and connection. Amazingly enough, I always feel the support of my classmates, professors and the dean. They have become part of my extended family.
You only not gain expertise in Health Informatics, but also lifelong friendships with other people who share your same passions and drives.
Imelda Soledad is a registered nurse and bone marrow transplant coordinator for Mount Sinai Medical Center. She is earning her Masters in Applied Health Informatics from Fordham.
Through the Looking Glass: One Student's Perspective on the Oxford Residency

By Matthew Sutfin
The bus from Heathrow Airport to Oxford is a surreal one: quotidian towns, gray highways, the errant farm or two, and then, a University that is twice as old as the United States and has the architecture to prove it. Suddenly, you realize that the opportunity of studying in Oxford isn't just a dream, but your reality. All you can do is soak it in, that is, until you decide to grab your bags and head to the Porters Lodge on Queen’s Lane to check in and get the show on the road.

Helmed by the esteemed program head Dr. John Chelsom, Fordham AHI’s State of the Art of Health Informatics class (ran concurrently with the Global Open Source EHR workshop and Annual Summit) hosted at St. Edmund (Teddy) Hall is a whirlwind week of engaging seminars, fascinating keynote speakers, and amazing opportunities to connect with fellow students, professors, and health informatics professionals. Projects will have you thinking critically about the nascent technologies emerging in the health informatics field. My team of four got the chance to create an artificially intelligent chatbot that could provide helpful and verified pharmaceutical and health informatics information to prospective users in the healthcare space. While a week isn't a terribly long time to study and develop, the network of experts available help facilitate the projects and ensure that you present your best work.


Reflecting back, I am still amazed I was allowed the opportunity to study in Oxford. This school is history manifest, the most renowned in the world, and for good reason. However, beyond the thousand year old bricks that comprise the university walls and the weighty reputation diffused throughout them, the most rewarding part of the week was meeting other health informatics students and professors in the Fordham AHI program. It was a chance to connect with people from across the globe and be able to call them all new friends; a chance to share ideas and make memories, frequently at the dedicated college pub (imagine that in America!). I can only speak fondly about my time at Oxford, and eagerly look forward to any opportunities to return.
Matthew Sutfin is a Masters student in Fordham's AHI program and a Medical Assistant for Optum Urgent Care. He lives in Melville, N.Y.